Report Writing
10 GDP Practices to Prevent Clinical Documentation Errors
Improve your site's data quality. Learn how to implement good documentation practices in clinical research to satisfy audits and inspections.
Feb 13, 2026

In clinical research, a single documentation error can derail an entire study, compromise patient safety, or lead to regulatory rejection. Every case report form, source document, and audit trail tells a story that investigators, sponsors, and regulatory bodies must trust without question. As research teams increasingly turn to the best AI for report writing to streamline their documentation workflows, maintaining rigorous documentation practices in clinical research remains essential to ensure data integrity, regulatory compliance, and study credibility. This article delivers 10 GDP practices to prevent clinical documentation errors, offering practical strategies to strengthen your documentation processes and protect your research from costly mistakes.
Whether you're managing source data verification, preparing for site audits, or creating standard operating procedures, having the right support can transform your documentation approach. Otio serves as your AI research and writing partner, helping you organize protocols, generate accurate reports, and maintain consistency across all clinical documentation so you can focus on what matters most: conducting high-quality research.
Summary
Clinical documentation errors persist not because research teams lack competence, but because manual processes, time constraints, and fragmented systems create conditions that make mistakes inevitable. Each data transfer between systems introduces an opportunity for error, and when coordinators handle repeated manual transcription across disconnected platforms, small mistakes such as transposed dates or shifted decimal points slip through undetected.
Poor documentation practices can increase monitoring costs by 30-40% in studies without standardization. These unplanned expenses stem from extended site visits, additional queries, and follow-up monitoring required when incomplete records prevent efficient data verification. The cost spiral extends beyond monitoring to data management teams spending excessive time resolving queries, medical monitors conducting additional safety reviews, and regulatory affairs staff preparing lengthy agency responses that could have been avoided with better initial documentation.
Documentation errors often remain invisible for months or years until external audits expose them as systemic compliance failures. A 2018 analysis of clinical trial compliance found that even large studies involving 8,381 recruited patients face scrutiny when documentation practices fail to meet regulatory standards.
Real-time documentation at the point of activity is the most accurate factor. When coordinators enter patient vitals during the visit instead of hours later, they capture exact values without relying on memory reconstruction. The moment between observation and documentation eliminates the gap where details fade or merge with other encounters, a specificity that exists only in the immediate moment and cannot be reliably reconstructed retrospectively.
Centralized documentation repositories eliminate the arduous work of assembling complete records scattered across paper binders, electronic data capture systems, emails, and shared drives. Fragmented storage leads to missing evidence during audits and to transcription errors that multiply when teams manually compile information from disconnected sources.
AI research and writing partner addresses documentation fragmentation by centralizing research materials in a single workspace, where protocols, reports, and source documents connect automatically, eliminating transcription and formatting errors that result from manually compiling information across scattered systems.
Table of Contents
Why Clinical Documentation Errors Still Happen
Clinical documentation errors persist because research teams operate under conditions that make accuracy difficult to sustain. Manual processes, time constraints, and fragmented systems create environments where even experienced professionals make preventable mistakes. The gap isn't competence. It's infrastructure.
Manual Entry Creates Compounding Risk
Most clinical research documentation still happens by hand. Staff transcribe handwritten notes into electronic systems, copy data between spreadsheets, and piece together reports from multiple disconnected sources. Each transfer introduces an opportunity for error. When a coordinator rushes to enter patient visit data before the next appointment, small mistakes slip through. A decimal point shifts. A date gets transposed. A unit of measurement changes without anyone noticing. These aren't failures of attention. They're inevitable outcomes when humans serve as the interface between paper records and digital systems.
The Contemporaneous Documentation Gap
According to Candello's 2024 Benchmarking Report, documentation deficiencies remain a leading factor in malpractice claims, with inconsistencies often traced back to manual transcription gaps. The pattern appears across institutions: high-performing teams still struggle when their processes depend on repeated manual data handling.
Retrospective Documentation Erodes Accuracy
Documentation rarely happens in real time. Clinic days are filled with:
Patient interactions
Protocol procedures
Urgent requests
Staff take quick notes, intending to complete full records later. Hours pass. Sometimes days. Memory degrades fast. A coordinator who saw eight patients yesterday can't reliably recall which one reported mild nausea versus moderate nausea. Timeline details blur. The exact sequence of events becomes approximate rather than precise.
Recollection Bias and the Fading Memory Liability
This isn't laziness. It's triage. When patient care demands immediate attention, documentation becomes the task that waits. But waiting costs accuracy. By the time records get completed, critical details have already faded or merged with other encounters.
Version Control Chaos
Research documents live everywhere:
Local hard drives.
Shared network folders.
Email attachments.
Cloud storage.
USB backups
Multiple versions circulate simultaneously, and teams rarely verify they're working from the latest file. A research coordinator updates a consent form template on her laptop. A colleague is using an older version saved on the shared drive. Another team member references a copy attached to an email from three weeks ago. All three believe they're using the current document.
Version Control Drift and Protocol-to-Procedure Alignment
The fragmentation feels manageable until an audit reveals that submitted case report forms reference outdated protocol versions, or that consent documents lack required language added in recent amendments. Then teams realize their file management system wasn't a system at all.
Training Gaps Normalize Errors
Many research staff learn documentation through observation rather than structured training. They watch colleagues adopt local habits and assume those practices meet regulatory standards. Formal documentation training occurs infrequently, if at all. When incorrect practices become embedded in daily workflow, they feel normal. Everyone signs records the same way, so it must be right. Everyone uses the same abbreviations, so they must be acceptable. These assumptions persist until external auditors point out violations that have existed for months or years.
Institutional Memory and Workaround Risks
The challenge isn't willful noncompliance. It's that teams don't know what they don't know. Without regular training and systematic review, documentation practices drift away from regulatory requirements without anyone noticing.
Workload Pressure Forces Speed Over Precision
Clinical research staff:
Juggles patient visits
Regulatory submissions
Monitoring preparations
Protocol updates
Administrative tasks simultaneously
Documentation becomes one item on an overwhelming list. Under pressure, speed feels more important than thoroughness. A coordinator skips the second verification step because the next patient is waiting. A data manager approves entries without full review because the submission deadline is tomorrow. These aren't character flaws. They're rational responses to impossible workload expectations.
The Speed-Accuracy Trade-off and Priority Burnout
The result:
Incomplete entries
Missed data checks
Rushed signatures that should have triggered additional review
Quality suffers not because people don't care, but because they're forced to choose among competing priorities with insufficient time to do it all.
Information Silos Block Verification
Research data scatters across:
Electronic data capture systems
Paper source documents
Email correspondence
PDF reports
Excel spreadsheets
Audio or video recordings
No single repository contains everything needed to verify a complete record. When an auditor requests documentation supporting a specific data point, staff search across multiple systems. The original measurement might be in a paper lab report. The transcription appears in the EDC. The explanation for a discrepancy lives in an email thread. The correction documentation is a scanned PDF in the folder labeled “Misc 2023.”
Fragmented Data as a Barrier to Audit-Ready Traceability
This fragmentation makes verification exhausting and error-prone. Teams can't easily cross-reference information or spot inconsistencies when relevant data is spread across five different places. Missing references and unsupported entries become inevitable. Platforms like Otio address this by centralizing research documentation in one workspace where teams can:
Organize protocols
Extract key information from multiple sources
Maintain searchable records that connect related documents
Instead of hunting across systems, researchers work from a single source that preserves context and enables quick verification.
Overconfidence in Good Enough
Most teams believe their documentation is adequate until an audit proves otherwise. Minor inconsistencies seem harmless. Small gaps feel insignificant. No one expects serious regulatory consequences from issues that appear trivial. This confidence isn't arrogance. It's a lack of perspective. Teams don't see patterns across their documentation because they review records individually, case by case. They miss systemic weaknesses that become obvious only when an external reviewer examines hundreds of entries together. By the time problems surface, they've accumulated into compliance risks that require extensive remediation. What felt “mostly fine” has fundamental gaps that threaten study integrity.
The System Problem
Documentation errors don't stem from careless individuals. They emerge from weak systems that make accuracy difficult and mistakes easy. Manual processes, delayed entry, poor version control, inconsistent training, excessive workload, fragmented storage, and unchecked confidence combine to create environments where errors become routine.
The Cost of Silent Data Integrity Failures
Skilled professionals work within these broken systems and still produce flawed documentation. The solution isn't working harder. It's building infrastructure that makes good documentation the natural outcome rather than a heroic effort. But understanding why errors happen is only half the picture. The real question is what those errors actually cost when they go undetected.
Related Reading
The Hidden Risk of Poor Documentation in Clinical Research
Documentation errors don't announce themselves. Most slip past unnoticed for weeks, months, sometimes years.
Teams continue working.
Studies progress.
Submissions move forward.
Then an audit or regulatory inspection occurs, and those invisible gaps suddenly become very visible problems.
The pattern repeats across research sites: small documentation inconsistencies accumulate quietly until external review exposes them as systemic compliance failures. By then, the damage extends far beyond paperwork.
Small Errors Become Major Audit Findings
A missing date on a consent form seems trivial. An unsigned lab report appears to be an administrative oversight. A corrected value without written justification appears to be a simple fix. Individually, these appear minor. Collectively, they signal pattern failures that regulators take seriously. According to a 2018 analysis of clinical trial compliance, even large studies involving 8,381 patients recruited can face scrutiny when documentation practices fail to meet regulatory standards. The size of the study doesn't protect against findings. In fact, larger trials often magnify documentation weaknesses because inconsistencies multiply across sites and patient visits.
The Not Documented, Not Done Enforcement Surge
Research teams often believe regulators focus primarily on scientific outcomes and patient safety protocols. Documentation feels secondary compared to the complexity of:
Trial design
Statistical analysis
Clinical procedures
This assumption creates vulnerability. FDA and EMA inspection reports consistently cite documentation deficiencies as a leading cause of compliance observations. Incomplete source data, inadequate audit trails, and missing contemporaneous records appear repeatedly in warning letters and inspection summaries. What teams dismiss as paperwork issues, regulators classify as data integrity failures.
The Hidden Cost of Reactive Compliance
When inspectors find patterns of poor documentation, they question everything.
If consent forms lack proper dates, can you prove that informed consent occurred before the procedures?
If source documents show corrections without explanation, how do you verify data accuracy?
If signatures appear inconsistent, who actually reviewed what?
Minor lapses escalate into formal observations that require corrective action plans, follow-up inspections, and extensive remediation, consuming months of staff time.
Delayed Submissions and Regulatory Rejections
Inconsistent documentation creates submission bottlenecks that teams rarely anticipate. Files get returned for clarification. Queries pile up. Database locks get postponed. Timelines that looked achievable suddenly stretch into extended delays. The problem compounds in multicenter trials where documentation practices vary across sites. One site maintains meticulous records. Another uses abbreviated notes. A third struggles with version control. When data management tries to reconcile these differences during database lock, discrepancies surface that require site-by-site resolution.
Why Clean Data Can't be Rushed
A study targeting a six-month submission window, during final review:
Finds that three sites have incomplete source verification
Two sites use outdated case report forms
Multiple patient visits lack contemporaneous documentation
The database lock, planned for March, won't occur until May. The regulatory submission has been moved from Q2 to Q3. Product launch timelines slip accordingly. These delays aren't random bad luck. They're predictable outcomes when documentation standardization gets deprioritized during study execution. Teams assume they can “clean up” records later, not realizing that retrospective fixes require exponentially more effort than maintaining quality from the start.
The Technical Validation Hurdle in Global Submissions
Industry compliance analyses show documentation quality significantly impacts submission timelines, particularly in complex trials spanning multiple countries and regulatory jurisdictions. What appears to be a normal regulatory review delay often stems from preventable documentation gaps that trigger additional scrutiny.
Increased Monitoring and Operational Costs
Poor documentation doesn't just create compliance risk. It increases operational expenses in ways that rarely surface in initial budget planning. When monitors arrive for site visits and discover incomplete records, they can't verify data accuracy efficiently. What should take two days stretches to four. Follow-up visits get scheduled. Additional queries get issued. Each extension adds monitoring costs that weren't budgeted.
The Correction Rework Loop and Monitoring Efficiency
Clinical operations research indicates that poor data quality can increase monitoring costs by 30 to 40 percent in studies where documentation practices lack standardization. These aren't abstract percentages. They translate to tens of thousands of dollars in unplanned expenses for mid-sized trials, potentially hundreds of thousands for large multinational studies.
The Site Performance Metric and Future Feasibility
The cost spiral extends beyond monitoring.
Data management teams spend excessive time resolving queries that stem from unclear source documentation.
Medical monitors conduct additional safety reviews because adverse event records lack sufficient detail.
Regulatory affairs staff prepare lengthy responses to agency questions that could have been avoided with better initial documentation.
Sponsors notice these patterns. Sites that consistently generate high query rates and require extensive monitoring support become less attractive for future studies. What starts as documentation shortcuts to save time ultimately costs both money and reputation.
Loss of Data Credibility
Accurate data becomes suspect data when documentation can't prove its accuracy. This distinction matters more than most research teams realize. Regulators don't just evaluate whether reported results are correct. They assess whether the documentation trail demonstrates that those results are trustworthy.
Can you prove the data point was recorded contemporaneously?
Can you verify who collected it?
Can you trace every correction back to the source documentation and provide clear justification?
Why Retrospective Data is a Red Flag
ICH-GCP guidelines establish the ALCOA principles:
Data must be Attributable
Legible
Contemporaneous
Original
Accurate
These aren't bureaucratic preferences. They're fundamental requirements for data integrity. When documentation fails these standards, even scientifically valid findings become questionable. A trial shows promising efficacy results, but inspection reveals that many data points were entered into the electronic data capture system days or weeks after patient visits, with minimal source documentation to verify timing or accuracy. The science might be sound, but the documentation can't prove it. Regulators downgrade the findings or exclude data from sites with persistent documentation failures.
Reconstructing the Digital Thread
This scenario occurs more often than the published literature suggests. Studies are delayed, data are excluded, and sometimes entire sites are excluded from analysis because documentation practices cannot support the collected data. Teams working in fragmented systems face particular risk here. When source documents live in paper files, electronic entries exist in the EDC, and supporting information scatters across emails and shared drives, creating a coherent audit trail becomes nearly impossible. Verification requires hunting across multiple systems, and gaps inevitably emerge.
From Scattered Files to Knowledge Graphs
Otio addresses this fragmentation by centralizing research documentation in a single workspace where teams can:
Organize protocols
Source documents
Supporting materials together
Instead of reconstructing audit trails across disconnected systems, researchers maintain connected records that preserve relationships between documents, making verification straightforward and reducing credibility risk.
Institutional Reputation Damage
Compliance findings don't stay private. Regulatory agencies publish inspection reports. Sponsors share audit results internally. Word spreads through the clinical research community about which sites consistently struggle with documentation quality. Damage accumulates slowly, making it easy to underestimate. A site receives minor findings during one inspection. Six months later, another audit identifies similar issues. A year passes, and a third review shows the problems persist. None of these individually seems catastrophic, but together they establish a pattern.
Documentation as Site Equity
Sponsors making site selection decisions for new trials review historical performance data. Sites with repeated documentation findings get deprioritized. Study allocations decrease. Revenue declines. Staff positions become harder to justify. What started as “just documentation issues” has evolved into an existential threat to the research program's viability. I've watched research sites that were once preferred partners of major sponsors gradually lose standing because they couldn't resolve persistent documentation-quality issues. The clinical expertise remained strong. The patient recruitment capabilities stayed solid. But sponsors couldn't accept the compliance risk, so they moved studies elsewhere. Rebuilding a reputation after it's damaged takes years of demonstrated improvement. Prevention costs far less than recovery.
Legal and Ethical Exposure
Documentation serves as legal protection when questions arise about:
Study conduct
Patient safety
Regulatory compliance
Weak documentation removes that protection precisely when it's most needed.
If a patient experiences an unexpected adverse event and questions whether proper safety monitoring was in place, what does the documentation show?
If an allegation arises of a protocol deviation, can contemporaneous records demonstrate what actually happened?
If regulatory authorities investigate potential misconduct, does the paper trail support or undermine the site's position?
When Missing Notes Become Evidence
Poor documentation creates ambiguity, and ambiguity creates legal vulnerability. When records are incomplete, retrospectively completed, or inconsistently maintained, defending against allegations becomes exponentially harder regardless of what actually occurred. Research institutions face regulatory sanctions, litigation risk, and potential loss of authority to conduct clinical trials when documentation failures suggest broader compliance problems. These consequences extend far beyond individual studies, affecting entire research programs.
Scientific Validity as an Ethical Imperative
The ethical dimension matters too. Clinical research exists to generate reliable evidence that improves patient care. When documentation practices compromise data integrity, the research fails to meet its fundamental purpose, even if no intentional misconduct occurred. Poor documentation doesn't just create compliance risk. It undermines the ethical foundation of the research enterprise.
Why These Risks Stay Hidden
Most research sites operate for extended periods without major compliance incidents.
Studies complete.
Data gets submitted.
Approvals happen.
This track record creates a false sense of confidence that current practices are adequate. The problem with compliance risk is that it operates on probability, not certainty. Weak documentation practices may not cause immediate problems; issues may not appear for months or years. Then a surprise inspection happens, or a sponsor conducts a for-cause audit, or a regulatory agency selects the study for detailed review. Suddenly, vulnerabilities that seemed theoretical become very real consequences.
Normalcy Bias and the Invisible Documentation Debt
Teams tell themselves the documentation is “good enough” because nothing bad has happened yet. They believe regulators won't scrutinize minor details. They assume they'll have time to fix issues if problems surface. These beliefs seem reasonable based on past experience, but they overlook how quickly situations can escalate when documentation failures are exposed during formal review. The gap between perceived risk and actual risk persists because feedback comes slowly and intermittently. Unlike clinical errors that produce immediate, visible consequences, documentation failures often remain invisible until external audits surface them.
Related Reading
10 GDP Practices That Prevent Documentation Errors
1. Record Data Immediately at the Point of Activity
The moment between observation and documentation determines accuracy more than any other factor. When coordinators enter patient vitals during the visit instead of two hours later, they capture exact values without relying on memory reconstruction. When lab results are logged as soon as they arrive, rather than being batched for end-of-day entry, timing remains precise and verifiable.
Cognitive Load and the Reliability of Late Data
Real-time documentation eliminates the gap where details fade or merge with other encounters. A coordinator who saw six patients yesterday can't reliably distinguish between patients who reported dizziness upon standing and those who reported dizziness throughout the day. The specificity that regulators require exists only in the immediate moment of observation. Electronic systems that enable bedside or exam-room data entry eliminate the most common excuse for delayed documentation. When tools are available at the point of activity, "I'll enter it later" is no longer necessary. The work is done once, accurately, rather than twice with degraded precision.
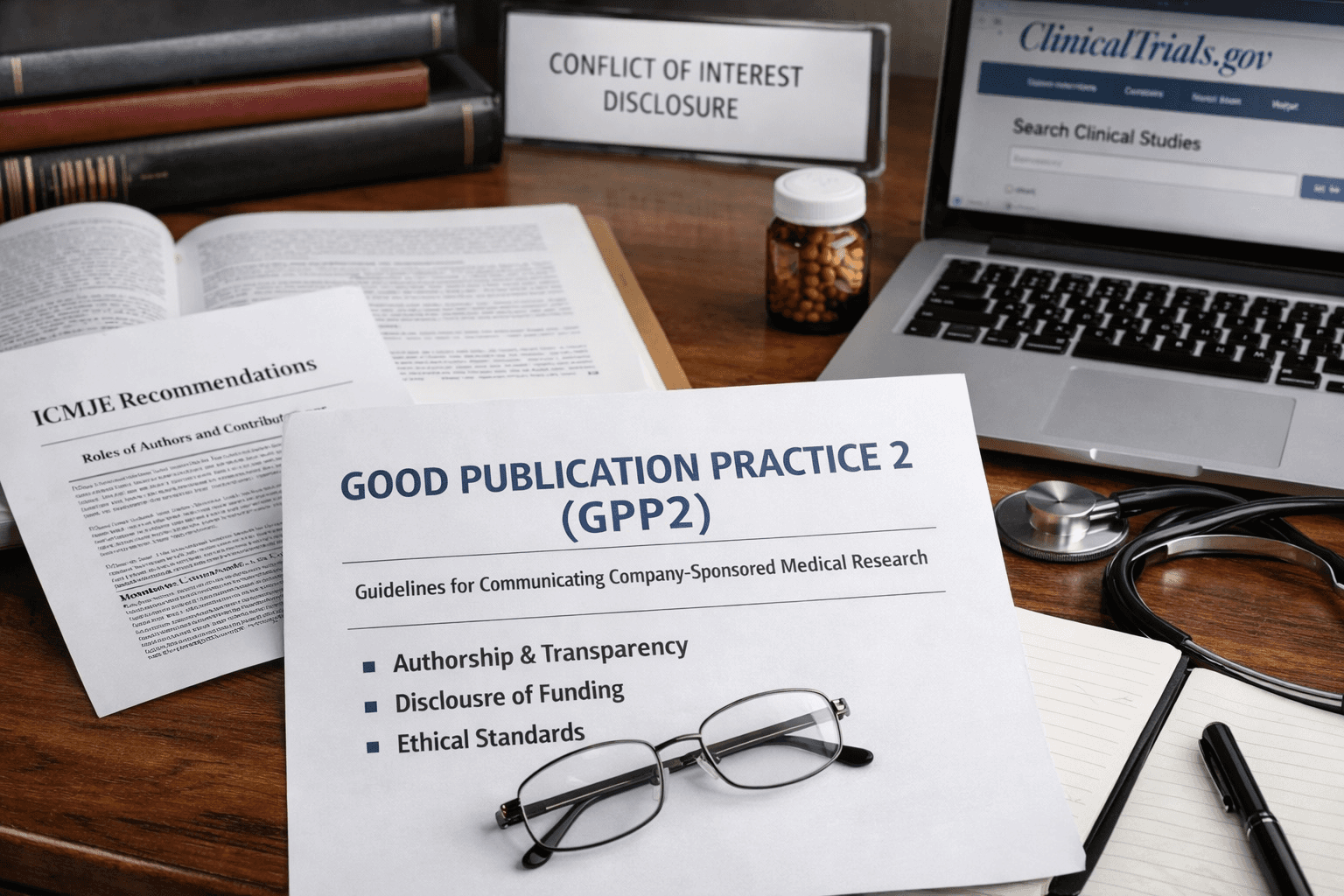
2. Follow ALCOA+ Documentation Principles
Regulators worldwide evaluate clinical research data using a consistent framework. ALCOA+ establishes that records must be:
Attributable
Legible
Contemporaneous
Original
Accurate
Complete
Consistent
Enduring
Available
These aren't bureaucratic preferences. They define what makes data legally defensible.
Attributable means that every entry can be traced to a specific person.
Legible means anyone can read it without interpretation.
Contemporaneous means documentation happens at the time of the activity, not reconstructed later.
Original means the first recording of information, not a copy or transcription.
Accurate means the record reflects what actually occurred.
Self-Auditing as a Survival Skill
Complete means all required information appears.
Consistent means data aligns across all related records.
Enduring means the record remains readable and intact over time.
Available means authorized personnel can access it when needed.
Sites that treat ALCOA+ as a checklist rather than abstract guidance catch problems before monitors arrive. When a coordinator reviews their day's documentation against these nine criteria, missing signatures and unclear abbreviations are immediately apparent, rather than months later during the audit.
3. Use Standardized Documentation Templates
Creating unique forms for each study increases the risk of omissions. When reviewing notes across protocols, coordinators must remember which fields matter for each study. This cognitive load produces gaps. Standardized templates for:
Consent records
Adverse event documentation
Protocol deviation reports
Visit notes reduce variability
A coordinator completing their twentieth adverse event form using the same template makes fewer mistakes than one adapting to a new format each time.
How Templates Protect Your Decision-Making Bandwidth
The efficiency gain compounds over time. New staff learn a single system rather than five.
Quality checks become faster because reviewers know exactly where to find required elements.
Query resolution accelerates because everyone speaks the same documentation language.
Templates don't eliminate thinking. They eliminate the mental effort wasted on formatting decisions, freeing attention for the actual clinical observations that matter.
4. Maintain Clear Audit Trails
Every correction tells a story. The question is whether that story creates confidence or suspicion. When a data value changes and the record displays a single-line strikethrough with the initials, date, and a brief reason, auditors see transparency. When a value appears different from the source documents without explanation, they see potential manipulation. Audit trails demonstrate that changes occurred through the proper process rather than by convenience or concealment. Electronic systems that automatically log who modified what and when provide this protection by default. Paper systems require discipline:
Never erase
Never use correction fluid
Never overwrite
The Anatomy of a Trustworthy Correction
The habit matters more than the specific method. A team that consistently documents the reasoning behind every correction builds credibility. A team that treats corrections as administrative nuisances that don't require explanation builds suspicion. Regulators understand that clinical research involves legitimate corrections. Lab values get transcribed incorrectly. Protocol versions get updated. Patient information changes. What they won't accept is corrections that appear designed to hide rather than clarify.
5. Apply Strict Version Control
Multiple uncontrolled document versions create protocol deviations that teams don't discover until an audit. A coordinator uses a consent form saved to their desktop from three months ago, not realizing the version on the shared drive includes updated language required by the IRB. The patient signs outdated documentation. The site now has a reportable deviation that could have been prevented.
When Version Drift Becomes a Protocol Violation
Version control means that a single file exists in one location, clearly labeled with a version number and date. Older versions are moved to an archive folder, not deleted, but unmistakably marked as obsolete. When protocol amendments occur, the new version replaces the old version in the active folder immediately, not gradually over several days as people finish using printed copies. The discipline feels tedious until you watch a site spend forty hours reconciling which patients received which consent version because files lived in seven different locations with inconsistent naming. Prevention takes minutes. Remediation takes weeks.
6. Centralize All Study Documentation
Fragmented storage guarantees missing evidence. When source documents live in paper binders, electronic entries exist in the EDC, monitoring reports sit in email, and protocol deviations are scattered across shared drives, creating complete documentation for audit becomes a laborious process. Centralization means that a single secure repository holds all study-related materials. Not scattered across systems, not duplicated in multiple locations, not stored locally on individual computers. One place, organized consistently, accessible to authorized personnel.
Transcription Errors in Manual Compilation
Many teams struggle with documentation written hours later because they can't easily reference what happened during earlier visits. Files stored in scattered emails mean context gets lost. Missing signatures multiply when teams can't quickly verify what still needs to be completed. Platforms like Otio address this by centralizing research documentation in one workspace where teams:
Organize protocols
Extract key information from multiple sources
Maintain searchable records that connect related documents
Instead of hunting across systems, researchers work from a single source that preserves context and enables quick verification, reducing the transcription and formatting errors that come from manual compilation.
The ROI of Administrative Velocity
The efficiency gain extends beyond compliance.
When preparing for monitoring visits, coordinators spend minutes gathering materials instead of hours.
When responding to queries, the relevant context is stored alongside the questioned data point rather than buried in another system.
When training new staff, they learn a single location rather than navigating an undocumented maze of folders and drives.
7. Perform Routine Internal Reviews
Waiting for monitors to identify documentation problems means fixing issues under time pressure with limited options. Internal reviews catch the same problems earlier when correction is straightforward. Weekly or monthly documentation checks using compliance checklists reveal patterns. Three patient visits missing the coordinator's signature indicate a process breakdown, not an isolated oversight. Five adverse event reports lacking required follow-up documentation signal training gaps. These patterns become visible only through systematic review, not case-by-case examination.
Standardizing the 15-Minute Weekly Self-Audit
The reviews don't require hours. A fifteen-minute weekly review of the past week's documentation catches most issues while details remain fresh and corrections are simple. Delaying review until pre-monitoring preparation means problems have accumulated for months, and memories have faded. Sites that perform routine internal reviews report fewer monitoring findings, not because their staff makes fewer initial errors, but because errors get corrected before they become compliance issues. The difference between a minor internal correction and a formal finding often comes down to the timing of detection.
8. Control Access and Authorization
Unlimited access to study records creates accountability gaps. When anyone can edit any document, tracing who made specific changes becomes impossible. When staff retain system access after leaving the organization, unauthorized modifications remain undetected. Role-based access means coordinators can enter data but not approve the final database lock. Monitors can review records but not modify source documents. Principal investigators can sign off on reports but not alter underlying data entries. Each role has appropriate permissions, no more.
Audit Trails as Forensic Evidence
Password protection and access logs provide security but also serve as evidence. When an auditor questions a data change, access logs show exactly who had the ability to make that modification and when they accessed the system. Without these controls, proving data integrity becomes nearly impossible. The friction of access control feels unnecessary until you need to demonstrate that only authorized personnel could have modified specific records. Then it becomes the evidence that protects the entire study.
9. Train and Retrain Staff on GDP
Documentation quality isn't common sense. It's a learned skill that requires ongoing reinforcement. New staff learn by watching colleagues, which means incorrect practices spread unless formal training establishes standards. Regular GDP training using real audit examples shows staff what regulators actually scrutinize. Abstract principles about data integrity feel theoretical. Showing an actual FDA 483 observation about missing contemporaneous documentation makes the requirement concrete and memorable.
Navigating the Shift to ICH E6(R3)
Training shouldn't happen once at study start and never again. Quarterly refreshers help keep practices consistent as staff turnover occurs and new protocols are introduced. Updates after monitoring visits or audits address specific findings before they become patterns. The return on training investment is reflected in lower query rates and fewer audit findings. A site that spends two hours per quarter on GDP training typically saves dozens of hours in query resolution and remediation. The math favors prevention.
10. Use Technology to Reduce Manual Errors
Automation removes human error points that no amount of training can eliminate. Electronic data capture with built-in validation rules prevents impossible values from being entered. Required fields that won't allow form submission ensure completeness. Automatic timestamps prove contemporaneous documentation without relying on manual dating. The technology doesn't need to be complex. Simple validation that birth dates precede visit dates helps catch transcription errors. Drop-down menus that limit adverse event severity to standard terminology prevent inconsistent coding. Automated calculation of derived values removes arithmetic mistakes.
Protecting Clinical Judgment in an Automated Workflow
Some teams use tools like Otio to generate first-pass documentation from source materials and link it to evidence, reducing the transcription and formatting errors that come from manually compiling and summarizing records. The technology handles repetitive structuring work while humans focus on clinical judgment and interpretation. The goal isn't eliminating human involvement. It's eliminating mechanical tasks where humans add little value and frequently make errors. Let technology handle data validation, formatting consistency, and audit trail generation. Let people handle clinical assessment, protocol interpretation, and patient interaction.
How These Practices Work Together
Individual practices provide incremental improvement. Combined systematically, they create documentation environments where accuracy becomes automatic. Real-time entry ensures data freshness. ALCOA+ principles ensure regulatory compliance. Standardized templates ensure completeness. Audit trails ensure transparency. Version control ensures currency. Centralization ensures accessibility. Internal reviews ensure early detection. Access controls ensure security. Training ensures competency. Technology ensures consistency.
Moving from Human Effort to Systemic Reliability
The result isn't perfection. It's a system where errors become rare rather than routine, where corrections occur quietly rather than during a crisis, and where audit preparation takes days rather than months. Sites that implement these practices report audit findings reduced by more than half in one monitoring cycle. Not because their staff suddenly became more careful, but because the infrastructure no longer allowed careless mistakes to persist.
The Key Principle
Good documentation isn't extra work added to the research process. It's how the research process gets executed correctly from the start. When GDP becomes embedded in daily workflow rather than treated as compliance overhead, the distinction between “doing the work” and “documenting the work” disappears. They become the same activity, occurring simultaneously, producing records that require minimal correction because they were created correctly initially. The practices above don't require heroic effort or unusual discipline. They require systems that make good documentation the path of least resistance, instead of an additional burden. But knowing what to do matters only if you can implement it without disrupting ongoing studies.
Build an Error-Free Documentation System
Understanding GDP rules matters less than having infrastructure that makes violations difficult to commit. The practices outlined earlier work only when embedded into repeatable systems that function without constant supervision. This means moving from knowing what to do to building environments where correct documentation happens automatically.
Start With a Two-Week Foundation Audit
Before making any changes, identify where your current system is leaking accuracy. Spend two days reviewing recent case report forms, source documents, and monitoring reports. Look specifically for:
Missing dates
Unsigned entries
Corrections without explanation
Format inconsistencies across similar document types
Don't fix anything yet. Just map the pattern. This audit reveals whether your problems stem from individual mistakes or systemic gaps. If three different coordinators all forget signatures on consent forms, the issue isn't training. It's that your template doesn't force signature verification before the document gets filed. If adverse event reports lack follow-up documentation across multiple studies, your tracking system fails, not your staff.
Build Templates That Enforce Completeness
Generic forms invite omission. When a visit note template includes optional fields, some coordinators complete them, and others skip them. Auditors identify an inconsistency and question whether the missing information indicates incomplete documentation or procedures. Redesign templates to make required fields non-navigable. Electronic forms that won't submit until all mandatory fields are completed eliminate the most common documentation gaps. Paper forms with a clear visual hierarchy reduce oversight errors, such as:
Bold labels for required fields
Checkbox confirmations that all sections are complete
The template itself becomes quality control. A coordinator rushing through end-of-day documentation can't accidentally skip the adverse event assessment if the form literally won't save without it.
Centralize Everything in One Searchable Location
Fragmentation creates the documentation errors that consume hours during audit preparation. Assembling complete records for a single patient visit requires archaeological work when protocols:
Live in one folder
Consent forms in another
Lab reports in email
Monitoring correspondence in a shared drive
Missing pieces become inevitable. Most teams address this by creating elaborate folder structures and naming conventions. This helps marginally but still requires remembering where each document type belongs and manually maintaining organization as files accumulate. The cognitive load guarantees eventual breakdown.
Reclaiming the 1.8 Hours Lost to Information Fragmentation
Teams working across scattered systems face a different problem. They spend more time searching for context than actually documenting. A coordinator responding to a query about a patient visit from three months ago searches across multiple locations to reconstruct the event, often finding supporting documentation in an unexpected location.
Why Disconnected Systems Breed Transcription Errors
Tools like Otio address this by centralizing research materials in a single workspace, where documents automatically link to one another. Instead of manually organizing files across systems, teams upload protocols, reports, and source documents into a single searchable environment. When reviewing a case report form, the related protocol section, consent document, and source notes appear together without hunting. This eliminates transcription errors that occur when manually compiling information from disparate sources.
Automate What Humans Do Poorly
People excel at clinical judgment. They struggle with repetitive verification tasks that require perfect consistency across hundreds of entries. A coordinator reviewing their twentieth patient visit of the week will miss details that automated validation would catch instantly. Electronic data capture systems with built-in rules prevent impossible values. A birth date that occurs after the consent date is rejected before anyone wastes time investigating why the record appears incorrect. Required fields that block form submission ensure completeness without relying on memory. Automated timestamps prove contemporaneous documentation without manual date entry.
RBQM and the Automation of Compliance
The automation doesn't replace thinking.
It eliminates mechanical verification tasks that add minimal value while causing frequent errors.
Calculate derived values automatically.
Validate date sequences programmatically.
Generate audit trail entries without manual logging.
Let your staff focus on patient interaction and clinical assessment rather than on data validation mechanics.
Schedule Weekly Internal Documentation Checks
Waiting for monitors to identify problems means fixing issues under time pressure, with limited options and faded memories. Weekly internal reviews using simple checklists catch the same problems, and corrections remain straightforward. Assign someone (rotating responsibility works well) to spend fifteen minutes each week reviewing the past week's documentation against basic compliance criteria. All entries signed? Dates present and logical? Corrections properly documented? Source documents filed? The review doesn't require hours. It requires consistency.
Using Trend Analysis to Pre-empt Audit Findings
Patterns emerge quickly. If three consecutive weeks show missing coordinator initials on lab report filing, you've identified a process gap before it becomes a compliance finding. If your tracking system consistently receives adverse event follow-up documentation days late, it needs to be adjusted. Early detection converts potential audit findings into internal corrections that leave no regulatory trace.
Train Using Real Audit Examples
Abstract GDP principles feel theoretical until staff see actual consequences. Telling coordinators that contemporaneous documentation matters elicits nods and no change in behavior. Showing them an FDA 483 observation citing a lack of contemporaneous records at a site similar to theirs immediately captures their attention and prompts behavior change. Quarterly training sessions using real inspection reports and audit findings make requirements concrete. Redact identifying information while retaining the specific language regulators used. When staff read that an inspector questioned data integrity because corrections lacked justification, they understand why the two-sentence explanation they've been skipping actually matters.
Analyzing Real-World Data Exclusion Cases
The training shouldn't lecture. It should show. Walk through an actual case where missing documentation led to data exclusion. Demonstrate the correct way to handle the exact scenarios that produced findings at other sites. Provide staff with the specific language and format that meet regulatory expectations, not vague guidance on being thorough.
Your System is Ready When Documentation Feels Effortless
Good infrastructure makes compliance the path of least resistance. When entering data correctly takes less effort than entering it incorrectly, when complete documentation takes less time than incomplete documentation, and when finding supporting evidence takes seconds rather than minutes, your system works. The test isn't whether you can produce audit-ready records when preparing for inspection. It's whether your daily documentation already meets audit standards without special preparation. If pre-monitoring cleanup consumes days of staff time, your system still depends on heroic effort rather than solid infrastructure. Build systems where accuracy happens automatically. Then documentation stops feeling like compliance overhead and becomes simply how the work gets done.
Related Reading
Document Generation Tools
How To Use Ai For Literature Review
How To Write A Research Summary
How To Write A White Paper
Best Ai For Literature Review
Best Report Writing Software
How To Write An Executive Summary For A Research Paper
Best Software For Automating Document Templates



